Leads ECG Placement: 7 Critical Mistakes You Must Avoid Now
Understanding the correct leads ecg placement is crucial for accurate cardiac diagnosis. A small error can lead to misinterpretation, delayed treatment, or even life-threatening consequences. Let’s dive into the essentials every healthcare provider must know.
What Is Leads ECG Placement and Why It Matters

Electrocardiography (ECG or EKG) is a non-invasive diagnostic tool used to assess the electrical activity of the heart. The accuracy of an ECG reading depends heavily on the correct placement of the leads. Leads ecg placement refers to the precise positioning of electrodes on the patient’s body to capture consistent and reliable cardiac signals.
The Science Behind ECG Leads
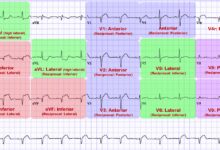
ECG machines use a system of 12 leads—comprising limb leads, augmented limb leads, and precordial (chest) leads—to view the heart’s electrical activity from multiple angles. Each lead provides a unique perspective, allowing clinicians to detect abnormalities such as arrhythmias, ischemia, or myocardial infarction.
- Limb leads (I, II, III) measure electrical activity in the frontal plane.
- Augmented limb leads (aVR, aVL, aVF) provide additional frontal plane views.
- Precordial leads (V1–V6) capture horizontal plane activity across the chest.
Incorrect leads ecg placement distorts these views, potentially mimicking pathology or masking real issues.
Clinical Consequences of Incorrect Placement
Errors in leads ecg placement are more common than many realize. Studies show that up to 40% of ECGs may have some degree of lead misplacement. This can result in:
- False diagnosis of myocardial infarction
- Misinterpretation of axis deviation
- Inaccurate assessment of chamber enlargement
- Unnecessary patient anxiety and further testing
“A misplaced ECG lead can look like a heart attack on paper—when the heart is perfectly fine.” — Dr. Emily Tran, Cardiologist at Johns Hopkins Medicine
Standard Leads ECG Placement: The 12-Lead System Explained
The 12-lead ECG is the gold standard for cardiac assessment. It requires 10 electrodes placed at specific anatomical landmarks. Mastery of leads ecg placement ensures that each lead records the correct vector of electrical activity.
Limb Lead Placement: Arms and Legs
The four limb leads are placed on the wrists and ankles (or upper arms and thighs in certain cases). The standard positions are:
- RA (Right Arm): On the right wrist or upper inner arm
- LA (Left Arm): On the left wrist or upper inner arm
- RL (Right Leg): On the right ankle or lower abdomen (ground electrode)
- LL (Left Leg): On the left ankle or upper inner thigh
These electrodes form the basis of the hexaxial reference system. Misplacement—even by a few centimeters—can alter the QRS axis significantly.
Precordial (Chest) Lead Placement: V1 to V6
The chest leads are placed in a specific sequence across the anterior thorax. Correct leads ecg placement here is vital for detecting anterior, lateral, and septal infarctions.
- V1: 4th intercostal space, right sternal border
- V2: 4th intercostal space, left sternal border
- V3: Midway between V2 and V4
- V4: 5th intercostal space, midclavicular line
- V5: Same horizontal level as V4, anterior axillary line
- V6: Same level as V4, midaxillary line
Errors in V1 and V2 placement are particularly common and can mimic right ventricular hypertrophy or Brugada pattern.
Common Errors in Leads ECG Placement and How to Avoid Them
Despite standardized guidelines, mistakes in leads ecg placement persist. Recognizing and correcting these errors is essential for diagnostic accuracy.
Misplacement of Chest Leads (Especially V1 and V2)
One of the most frequent errors is placing V1 and V2 too high or too lateral. This can shift the R-wave progression abnormally and mimic anterior myocardial infarction.
- Always count intercostal spaces from the angle of Louis (sternal angle) at the 2nd rib.
- Use anatomical landmarks, not estimation.
- Recheck placement if V1 and V2 show deep S-waves or absent R-waves.
A study published in NCBI found that incorrect V1/V2 placement occurred in over 30% of routine ECGs.
Reversal of Limb Leads
Limb lead reversal—especially LA/RA or LA/LL—is another common mistake. Right-arm/left-arm reversal can mimic dextrocardia or lead to incorrect axis interpretation.
- Check for inverted P waves in lead I.
- Look for positive deflections in aVR when they should be negative.
- Verify electrode colors: White (RA), Black (LA), Red (RL), Green (LL).
Lead reversals can be detected by analyzing lead I and aVR patterns. For example, if lead I shows inverted P, QRS, and T waves, suspect RA/LA reversal.
Incorrect Positioning of V4, V5, and V6
Placing V4 too high or too lateral affects lateral lead readings (V5, V6). This can mask lateral wall ischemia or create false ST-segment changes.
- Always locate the 5th intercostal space at the midclavicular line for V4.
- Ensure V5 and V6 are on the same horizontal plane as V4.
- Use a measuring tape for consistency in serial ECGs.
For patients with large breasts, lift the breast tissue to place V3–V6 correctly on the chest wall, not on the breast itself.
Special Considerations in Leads ECG Placement
Not all patients fit the standard anatomical model. Special populations require modifications in leads ecg placement while maintaining diagnostic integrity.
ECG Placement in Obese Patients
Excess adipose tissue can interfere with electrode contact and signal quality. In obese patients:
- Use adhesive electrodes with strong gel.
- Shave hair if necessary for better adhesion.
- Consider alternative limb lead placements (e.g., on upper arms/thighs instead of wrists/ankles).
- Ensure chest leads are placed on the chest wall, not on pannus or breast tissue.
Signal noise and poor R-wave progression are common issues in this population due to increased distance between heart and electrodes.
Leads ECG Placement in Women with Large Breasts
Improper placement under or on breast tissue can displace leads inferiorly and laterally, leading to false ECG findings.
- Lift the breast to locate the 4th and 5th intercostal spaces.
- Place V3–V6 on the chest wall, not on the breast.
- Use assistants if needed to maintain retraction during placement.
A study in European Heart Journal emphasized that up to 50% of ECGs in women had misplaced precordial leads, contributing to gender-based diagnostic disparities.
Pediatric and Neonatal ECG Placement
Children have smaller thoraxes and different heart positions. Leads ecg placement must be adjusted accordingly.
- Use smaller electrodes designed for pediatric patients.
- Place V4R (right-sided V4) in suspected right ventricular involvement.
- Adjust intercostal spacing based on body size.
In neonates, the right ventricle is more dominant, so R-waves in V1 are normally larger. Misplacement can exaggerate this, leading to false diagnosis of RVH.
Best Practices for Accurate Leads ECG Placement
Consistency, training, and attention to detail are key to ensuring correct leads ecg placement across all clinical settings.
Step-by-Step Guide to Proper Electrode Placement
Follow this standardized protocol to minimize errors:
- Explain the procedure to the patient and ensure they are lying flat and relaxed.
- Locate the angle of Louis (sternal angle) and count down to the 4th intercostal space for V1 and V2.
- Place V4 at the 5th ICS, midclavicular line.
- Place V3 midway between V2 and V4.
- Align V5 and V6 horizontally with V4 at the anterior and midaxillary lines.
- Attach limb leads to wrists and ankles (or upper arms/thighs if needed).
- Double-check all connections and lead labels before recording.
Using a checklist can reduce placement errors by up to 60%, according to research from the American Heart Association.
Training and Certification for Healthcare Providers
Regular training is essential. Many hospitals now require ECG competency certification for nurses and technicians.
- Conduct hands-on workshops with mannequins and real patients.
- Use ECG simulators to test lead placement knowledge.
- Implement peer review of ECG tracings to identify recurring errors.
Organizations like the American Association of Critical-Care Nurses (AACN) offer ECG interpretation and placement courses that improve clinical accuracy.
Use of Technology to Improve Accuracy
Modern ECG machines come with features to detect lead misplacement.
- Some devices provide real-time alerts for limb lead reversals.
- Digital ECGs allow for post-acquisition correction of lead placement artifacts.
- AI-powered systems can flag suspicious patterns suggestive of incorrect leads ecg placement.
While technology helps, it cannot replace proper initial placement. Always verify physical electrode positions before relying on software corrections.
Impact of Leads ECG Placement on Diagnosis and Treatment
The consequences of incorrect leads ecg placement extend beyond the ECG strip—they affect clinical decision-making and patient outcomes.
False Positives and Unnecessary Interventions
Misplaced leads can mimic ST-elevation myocardial infarction (STEMI), leading to unnecessary activation of the cath lab.
- Up to 15% of suspected STEMIs are later found to be ECG artifacts due to lead misplacement.
- Unnecessary angiograms expose patients to radiation and contrast risks.
- Hospital resources are wasted on false emergencies.
A case report in Journal of Electrocardiology described a patient mistakenly taken to the cath lab due to V1–V3 misplacement simulating anterior STEMI.
Missed Diagnoses Due to Lead Errors
Conversely, incorrect placement can mask real pathology.
- Lateral lead misplacement may hide ST elevations in circumflex artery occlusion.
- High chest lead placement can obscure inferior Q waves.
- Lead reversals may normalize an abnormal axis, delaying diagnosis of conduction disorders.
In one study, 12% of missed myocardial infarctions were linked to suboptimal ECG technique, including leads ecg placement errors.
Legal and Ethical Implications
Incorrect ECG interpretation due to poor lead placement can lead to malpractice claims.
- Failure to follow standard protocols may be seen as negligence.
- Hospitals may be held liable for diagnostic errors stemming from preventable technical flaws.
- Documentation of proper placement should be part of the ECG report.
“Standardization isn’t just best practice—it’s a legal safeguard.” — Legal expert Mark Delaney, Healthcare Law Review
Advanced Techniques and Modifications in Leads ECG Placement
Beyond the standard 12-lead ECG, specialized techniques require precise leads ecg placement for targeted diagnosis.
Right-Sided ECG (V4R) for Right Ventricular Infarction
In patients with inferior STEMI, right-sided leads can detect right ventricular involvement.
- Place V4R at the 5th intercostal space, midclavicular line on the right side.
- ST elevation in V4R is a strong predictor of RV infarction.
- Requires careful labeling to avoid confusion with standard leads.
Failure to perform right-sided ECG in suspected inferior MI can miss critical hemodynamic instability.
Posterior ECG Leads (V7–V9)
Posterior myocardial infarction may not show on standard leads. Posterior leads are essential in high-risk patients.
- V7: 5th ICS, left posterior axillary line
- V8: 5th ICS, left mid-scapular line
- V9: 5th ICS, left paraspinal area
ST elevation in V7–V9 confirms posterior MI, often associated with large infarcts and worse prognosis.
Esophageal and Intracardiac Leads
In electrophysiology studies, specialized leads are placed inside the heart or esophagus.
- Esophageal electrodes provide close proximity to the atria for arrhythmia monitoring.
- Intracardiac leads are used during ablation procedures.
- These require advanced training and are not part of routine leads ecg placement.
While not standard, understanding these modifications highlights the importance of spatial accuracy in cardiac monitoring.
Future Trends in Leads ECG Placement and Monitoring
As technology evolves, so do the methods and standards for leads ecg placement.
Wearable ECG Devices and Leadless Monitoring
Devices like the Apple Watch, AliveCor Kardia, and Zio Patch offer continuous monitoring with fewer or no traditional leads.
- These use 1- or 2-lead systems, limiting full 12-lead diagnostic capability.
- They are useful for rhythm screening but not for ischemia detection.
- Integration with AI allows for real-time arrhythmia detection.
However, they do not replace the need for proper leads ecg placement in acute settings.
AI and Machine Learning in ECG Interpretation
Artificial intelligence is being trained to detect lead misplacement automatically.
- Deep learning models can identify patterns of limb lead reversal or chest lead displacement.
- Some systems provide feedback before ECG interpretation.
- AI cannot correct physical errors—only flag them.
A 2023 study in Nature Medicine showed AI could detect lead errors with 92% accuracy, reducing false diagnoses.
Standardization and Global Guidelines
Organizations like the American Heart Association (AHA), European Society of Cardiology (ESC), and Heart Rhythm Society (HRS) continue to refine ECG standards.
- Harmonizing electrode color codes globally (IEC 60601-2-25).
- Promoting universal training modules.
- Advocating for mandatory ECG competency in medical education.
Future guidelines may include mandatory photo documentation of lead placement for high-stakes ECGs.
What is the correct placement for ECG lead V1?
V1 should be placed in the 4th intercostal space at the right sternal border. This is a critical landmark for accurate precordial lead recording and proper R-wave progression analysis.
What happens if limb leads are reversed during ECG?
Limb lead reversal can cause significant ECG abnormalities, such as inverted P waves in lead I (RA/LA reversal) or mimic dextrocardia. It can lead to incorrect axis determination and misdiagnosis of cardiac conditions.
How can I ensure accurate leads ECG placement in female patients?
In female patients, especially with large breasts, lift the breast tissue to place V3–V6 directly on the chest wall at the correct intercostal spaces. Never place electrodes on breast tissue, as this displaces leads and distorts readings.
Can wearable devices replace standard 12-lead ECG placement?
No, wearable devices cannot fully replace standard 12-lead ECGs. While useful for rhythm monitoring, they lack the multi-angle views needed to diagnose ischemia, infarction, or chamber abnormalities accurately.
What are the consequences of incorrect precordial lead placement?
Incorrect precordial lead placement can mimic or mask myocardial infarction, alter R-wave progression, and lead to misdiagnosis of ventricular hypertrophy or ischemia. It may result in unnecessary interventions or missed critical conditions.
Accurate leads ecg placement is not just a technical step—it’s a cornerstone of cardiac diagnosis. From proper limb and chest electrode positioning to understanding the impact of errors, every detail matters. By following standardized protocols, investing in training, and leveraging technology, healthcare providers can ensure reliable ECG results. Whether in emergency rooms, clinics, or remote monitoring, precision in leads ecg placement saves lives by preventing misdiagnosis and guiding appropriate treatment. As medicine advances, the fundamentals remain unchanged: correct placement leads to correct decisions.
Further Reading: